Women & Sleep: Needs, Disorders, & Recommendations
An overview of various sleep problems that affect women more
Good sleep is essential for our physical, mental, and emotional wellbeing. The average adult needs at least seven hours of sleep each night. Unfortunately, fewer than two-thirds of women actually get that much sleep each night, according to the CDC.
Biological conditions unique to women, like the menstrual cycle, pregnancy and menopause, all affect how well a woman sleeps. Women experience changing levels of hormones , like estrogen and progesterone, throughout the month and over her lifetime. Understanding the effects of these hormones, environmental factors, and lifestyle habits can help women enjoy a good night’s sleep.

How Much Sleep Do Women Need?
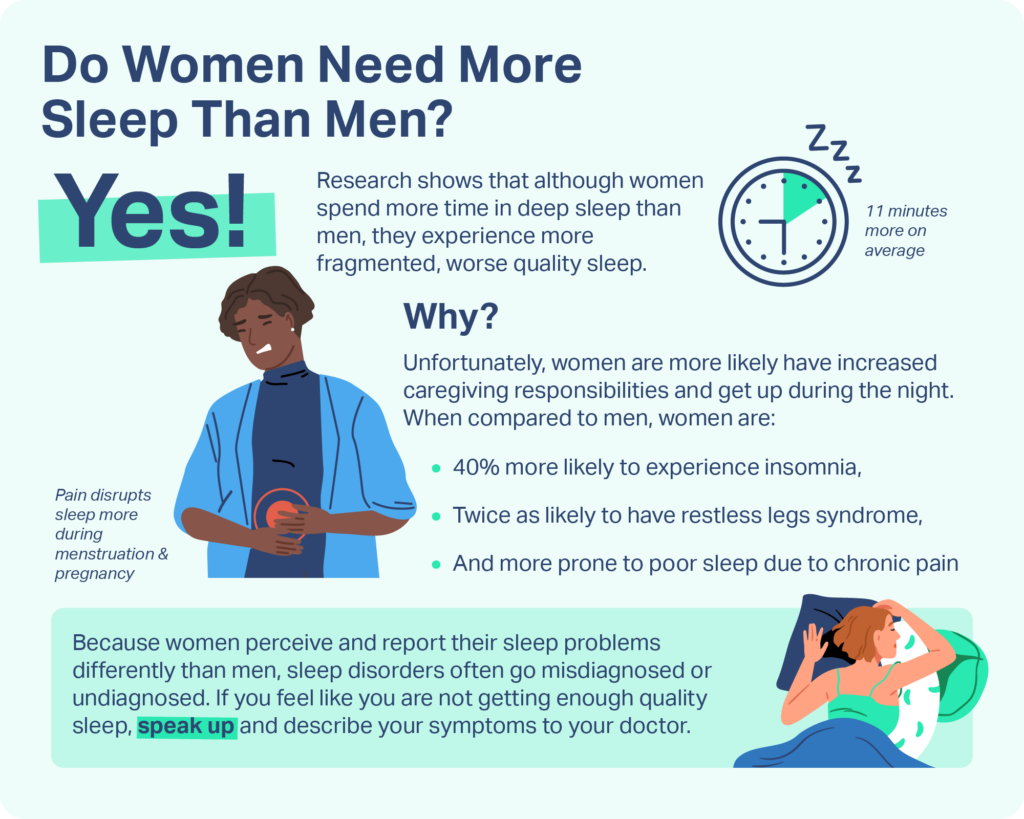
The average adult woman sleeps eight hours and 27 minutes per night. Studies show that women tend to sleep approximately 11 minutes more than men, despite having less time for sleep due to differences in paid and unpaid work, increased caregiving responsibilities, and family and social roles.
However, despite getting more sleep overall, researchers found that women experience lower-quality sleep than men. One reason could be that women are more likely to get up to take care of others, interrupting their sleep. Women are also more likely to nap during the day, which can further disrupt their sleep quality at night.
Common Sleep Problems for Women
70 million Americans suffer from sleep problems, but men and women don’t suffer equally. Women are more likely to have sleep problems than men. Women are also more prone than men to develop certain sleep disorders, including insomnia and restless legs syndrome.
Below we review the most common sleep issues that affect women.
Insomnia
People with insomnia regularly have difficulty falling or staying asleep. As a result, they don’t feel refreshed upon waking up and have difficulty functioning during the day. Insomnia is the most common sleep disorder, but women are 40 percent more likely to suffer from it than men.
Women may be more likely to experience insomnia for a number of reasons. Hormonal changes associated with menstruation, pregnancy, and menopause can alter a woman’s circadian rhythm, and consequently contribute to sleeplessness. The prevalence of insomnia among women increases significantly in older age, as they transition through menopause. Hot flashes and night sweats disrupt sleep, and are experienced by 75 to 85 percent of women with menopause. Women are also nearly twice as likely as men to report depression and anxiety — two conditions which are closely connected with insomnia.
Treatment for insomnia often begins with better sleep habits, such as following a regular sleep schedule, reducing one’s caffeine and alcohol intake, and improving the sleep environment. If an underlying condition is contributing to insomnia — such as depression, bladder problems, or pain — a doctor may focus on treating that first through medication, therapy, and lifestyle changes.
Pain and Sleep
Pain is strongly associated with insomnia . Pain makes it difficult to get comfortable enough to fall asleep. It also makes it challenging to stay asleep, as certain conditions may force you to readjust during the night to avoid waking up in pain. Some conditions associated with chronic pain are more common among women , including migraine, tension headaches, heartburn, arthritis, and fibromyalgia.
Treatment for pain-related sleep problems may focus on the source of pain, the sleeping difficulty, or both. A combination of relaxation techniques, cognitive behavioral therapy, lifestyle changes, and over-the-counter and prescription medications may help.
Nocturnal Sleep-Related Eating Disorder (NS-RED)
Nocturnal sleep-related eating disorder (NS-RED) is a parasomnia where individuals eat food during the night while they are asleep, and have no recollection of it upon waking up. Women are significantly more likely to have NS-RED. NS-RED can occur during sleepwalking and may coexist with other sleep disorders that trigger sleep eating.
NS-RED can be treated with medication, therapy, stress management techniques, and lifestyle changes, such as limiting caffeine and alcohol.
Restless Legs Syndrome (RLS) and Periodic Limb Movement Disorder (PLMD)
Restless legs syndrome (RLS) causes unpleasant crawling and tingling sensations in the legs, which occur when lying down and are accompanied by an uncontrollable urge to move the legs. Because symptoms occur when lying down and can only be relieved through movement, many women with RLS have difficulty sleeping. These sleep issues can lead to daytime sleepiness, mood swings, anxiety and depression — all of which can worsen sleep problems in turn.
Women are twice as likely as men to have RLS, and more likely to experience comorbidities than men. The risk for RLS is higher among women with multiple children, and increases twofold from pregnancy to menopause.
Iron deficiency , which is more common in women, may be a risk factor for RLS. Treatment may include iron supplements, other medications, and lifestyle changes to improve sleep.
Shift Work and Sleep
Nearly 15 million Americans work non-traditional hours, outside of the normal 9 a.m. to 5 p.m. Shift workers, especially those who work the night shift, often have to sleep at non-traditional hours. This causes disruptions to their natural sleep-wake cycle, with ramifications that can lead to less restful sleep, less sleep overall, and more sleep-related accidents and illnesses. Irregular work schedules can also put strain on family and social life, which can lead to stress and other emotional problems that worsen sleep.
For example, one large study found that female night shift workers have a significantly greater risk of developing breast cancer and cardiovascular disease . They are also more likely to have irregular menstrual cycles . While further research is necessary, scientists believe the changes in exposure to light and lost sleep caused by shift work may have biological or hormonal effects that disrupt the sleep-wake cycle.
Light therapy, medication, and lifestyle changes may be proposed as treatment. Women experiencing sleep issues and other problems due to shift work should consult a doctor.
Sleep Apnea
Sleep apnea is a sleep disorder characterized by temporary pauses in breathing during sleep. These pauses cause loud snoring, choking, and gasping sounds that disrupt sleep and lead to excessive daytime sleepiness. Sleep apnea is twice as common in men, although it increases in women after age 50.
Obesity and older age are the two largest risk factors for sleep apnea. During menopause, women experience hormonal changes that trigger an increase in abdominal fat, as well as lower progesterone levels . Both of these may explain their increased risk of sleep apnea.
Women who believe they have sleep apnea should consult a doctor. A number of effective treatment options are available, including CPAP therapy. Hormonal replacement therapy for menopause may lower their risk, as can changing their diet and exercise.
How Sleep Changes Throughout a Woman’s Life
Biological differences explain some of the sleep differences between women and men. Women tend to take longer to fall asleep, and to spend more time in restorative slow-wave deep sleep than men.
The gender differences in sleep emerge in puberty. Among high school students, females are significantly less likely to get their recommended eight hours of sleep per night than their male counterparts. They are also more likely to have comorbid depression. These sleep issues persist at other major hormonal transitions in a woman’s life, such as menstruation, pregnancy, and menopause.
One-third of women experience cramps, headaches, and bloating that cause sleep disturbances during their menstrual cycle. And even though total sleep time stays roughly the same throughout the menstrual cycle, women are most likely to report lower sleep quality in the week before their period. It’s also during this time that women with severe PMS more frequently report disturbing dreams, sleepiness, fatigue, and trouble concentrating.
Women are more likely to have sleep troubles during pregnancy, especially during their third trimester when symptoms of RLS, OSA, pain, and incontinence are more frequent. Sleep disruptions continue into postpartum, when hormone levels drop. This sudden change in hormones, along with raising a newborn, can worsen sleep quality and daytime sleepiness.
Final Takeaway to Remember
Women perceive and report their sleep problems differently than men. For example, women who seek treatment for sleep apnea are more likely to focus on symptoms like fatigue and depression, whereas men will describe snoring and gasping. This may lead to fewer women being diagnosed , or to a misdiagnosis of insomnia when sleep apnea is the underlying condition.
Sleep problems should not be taken lightly. Consult with your doctor if you notice any concerning symptoms and feel like your sleep is affecting your quality of life.
Sleep issues may change or vary in intensity throughout life, but there is hope for better sleep. Start with better sleep hygiene. Limit your caffeine, alcohol, and nicotine intake and eat a well-balanced diet. Engage in regular exercise and follow a consistent sleep schedule, even on weekends. Finally, make your bedroom as cool, dark, and quiet as possible — and remove the clutter and electronics — so your bedroom is the ideal environment for sleep.
References
18 Sources
-
Nowakowski, S., Meers, J., & Heimbach, E. (2013). Sleep and women’s health. Sleep Medicine Research, 4(1), 1–22.
https://pubmed.ncbi.nlm.nih.gov/25688329/ -
Burgard, S. A., & Ailshire, J. A. (2013). Gender and Time for Sleep among U.S. Adults. American sociological review, 78(1), 51–69.
https://pubmed.ncbi.nlm.nih.gov/25237206/ -
Centers for Disease Control and Prevention. (2017b, June 5). CDC – About Our Program – Sleep and Sleep Disorders. CDC.gov.
https://www.cdc.gov/sleep/about_us.html -
Mallampalli, M. P., & Carter, C. L. (2014). Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. Journal of women’s health (2002), 23(7), 553–562.
https://pubmed.ncbi.nlm.nih.gov/24956068/ -
Moline, M. L., Broch, L., Zak, R., & Gross, V. (2003). Sleep in women across the life cycle from adulthood through menopause. Sleep medicine reviews, 7(2), 155–177.
https://linkinghub.elsevier.com/retrieve/pii/S108707920190228X -
Pinkerton, J. V. (2019, December). Menopause. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/women-s-health-issues/menopause/menopause -
Albert P. R. (2015). Why is depression more prevalent in women?. Journal of Psychiatry & Neuroscience, 40(4), 219–221.
https://pubmed.ncbi.nlm.nih.gov/26107348/ -
McLean, C. P., Asnaani, A., Litz, B. T., & Hofmann, S. G. (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035.
https://pubmed.ncbi.nlm.nih.gov/21439576/ -
Swanson, L. M., Pickett, S. M., Flynn, H., & Armitage, R. (2011). Relationships among depression, anxiety, and insomnia symptoms in perinatal women seeking mental health treatment. Journal of women’s health (2002), 20(4), 553–558.
http://www.liebertpub.com/doi/10.1089/jwh.2010.2371 -
Finan, P. H., Goodin, B. R., & Smith, M. T. (2013). The association of sleep and pain: An update and a path forward. The Journal of Pain, 14(12), 1539–1552.
https://pubmed.ncbi.nlm.nih.gov/24290442/ -
The Office on Women’s Health. (2017). Insomnia | Womenshealth.gov. Womenshealth.Gov.
https://www.womenshealth.gov/a-z-topics/insomnia -
Winkelman J. W. (1998). Clinical and polysomnographic features of sleep-related eating disorder. The Journal of clinical psychiatry, 59(1), 14–19.
https://pubmed.ncbi.nlm.nih.gov/9491060/ -
Allen, R. P., Auerbach, S., Bahrain, H., Auerbach, M., & Earley, C. J. (2013). The prevalence and impact of restless legs syndrome on patients with iron deficiency anemia. American journal of hematology, 88(4), 261–264.
https://onlinelibrary.wiley.com/doi/10.1002/ajh.23397 -
Centers for Disease Control and Prevention. (2018, August 29). Work Schedules: Shift Work and Long Hours | NIOSH | CDC. CDC.gov.
https://www.cdc.gov/niosh/topics/workschedules/default.html -
Chung, S. A., Wolf, T. K., & Shapiro, C. M. (2009). Sleep and health consequences of shift work in women. Journal of women’s health (2002), 18(7), 965–977.
http://www.liebertpub.com/doi/10.1089/jwh.2007.0742 -
Baker, F. C., & Driver, H. S. (2007). Circadian rhythms, sleep, and the menstrual cycle. Sleep medicine, 8(6), 613–622.
https://linkinghub.elsevier.com/retrieve/pii/S1389945706006216 -
Ruchała, M., Bromińska, B., Cyrańska-Chyrek, E., Kuźnar-Kamińska, B., Kostrzewska, M., & Batura-Gabryel, H. (2017). Obstructive sleep apnea and hormones – a novel insight. Archives of medical science : AMS, 13(4), 875–884.
https://pubmed.ncbi.nlm.nih.gov/28721156/ -
Wimms, A., Woehrle, H., Ketheeswaran, S., Ramanan, D., & Armitstead, J. (2016). Obstructive Sleep Apnea in Women: Specific Issues and Interventions. BioMed research international, 2016, 1764837.
https://pubmed.ncbi.nlm.nih.gov/27699167/









