How to Sleep Better While Pregnant
Sleep deprivation is an inevitable reality for new parents. Unfortunately for most, sleep troubles start before the baby is even born. as fluctuating hormones, changing body systems, and stress levels fuel a host of physiological shifts during pregnancy. As a result, its common to experience nighttime awakenings, insomnia, poor sleep quality, and excessive daytime fatigue throughout all three trimesters.
Sufficient shut-eye is critical for both developing babies and mothers. Inadequate sleep may increase the risk of preterm birth and postpartum depression , excess pregnancy weight gain , and contribute to elevated body mass index and high blood pressure in the newborn .
There are many strategies for mitigating sleep disruptors and getting the rest that you and your baby need.
Find a Comfortable Position
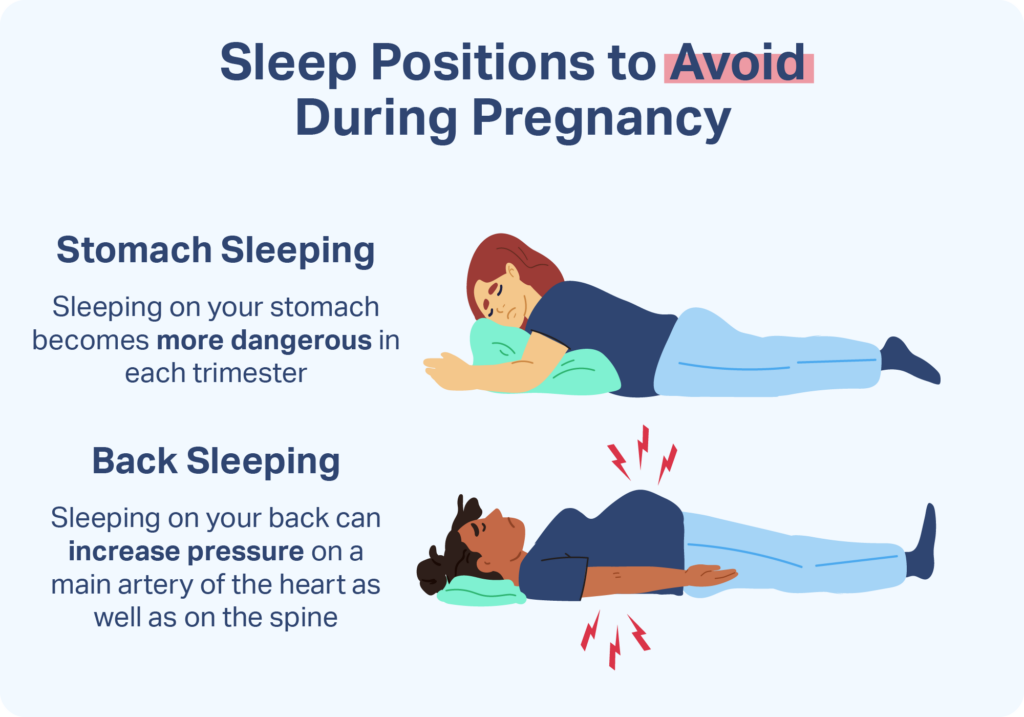
As the unborn baby grows larger, a pregnant woman might have difficulty finding a comfortable sleeping position. Expectant mothers should be aware some experts advise to avoid sleeping flat on their back, which can compress the inferior vena cava and decrease oxygen to the placenta .

Pregnant women are frequently most comfortable sleeping on their side with bent knees, which promotes healthy circulation. Most doctors recommend sleeping on the left side specifically, as this position is thought to protect the liver and increase blood flow to the heart, fetus, uterus, and kidneys.
These techniques can make side sleeping more comfortable:
- Place a pillow under your baby bump or between your legs.
- Use a rolled up blanket at the small of your back to relieve pressure.
- Try a foam or egg crate mattress pad to ease sore hips.
- Use extra pillows or a body pillow to support your body.
If you revert to sleeping on your back, don’t panic. It’s common for pregnant women to spend at least some time sleeping this way. If you are prone to this position, try placing a wedge pillow behind you when you go to sleep on your side. That way, should you roll back, you’ll at least be at a tilt, thereby lessening the effect of sleeping on your back.
Eat and Drink Strategically
During gestation, hormonal changes combined with an expanding uterus cause the entire digestive system to slow down. This can cause constipation, indigestion, and heartburn, which might become worse at night. At the same time, increased kidney productivity and pressure on the bladder from the growing baby make urination more frequent. Managing the body’s digestive input and output is crucial for a good night’s sleep.
Try these dietary changes to potentially avoid sleep disruptions:
- Avoid carbonated drinks, citrus, peppermint, tomatoes, and spicy or fatty foods. These can trigger acid reflux .
- Refrain from eating within three to four hours of bedtime.
- Eat small meals throughout the day, instead of three large meals.
- Don’t drink liquid during meals or within two hours of bed.
- Cut out caffeine. This is a stimulant that keeps you awake, and can be harmful for developing babies .
Improve Your Sleep Hygiene
Sleep hygiene is a collection of habits and behaviors that promote reliable, quality sleep. Sleep hygiene is important for everyone, and can make a big difference during pregnancy.
Improve your sleeping habits with these strategies:
- Go to bed and get up at the same time each day.
- Use your bed only for sleeping and sex.
- Don’t exercise within three hours of bedtime.
- Keep electronics out of the bedroom, and avoid screens before bed.
- If you can’t sleep within 30 minutes, get up and do a non-stimulating activity like reading.
Ensure Healthy Breathing
Weight gain, along with hormonal and physiological changes, predispose pregnant women to sleep disordered breathing (SDB). The most common manifestations of SDB during pregnancy include snoring and obstructive sleep apnea, a condition in which the airway becomes repeatedly blocked during sleep.
Getting a handle on SDB is crucial because this condition has been associated with adverse maternal and fetal outcomes , raising the risk of preeclampsia, hypertension, and gestational diabetes. Unchecked SDB can negatively affect overall quality of life, leading to excessive daytime sleepiness, morning headaches, and cognitive impairment. Fortunately, evidence suggests that treating even mild SDB improves the health of mother and baby.
To breathe well at night, it may help to:
- Mitigate pregnancy weight gain, with the guidance of your obstetrician. Excess weight is one of the main causes of SDB.
- Consider using a humidifier. Nasal congestion, which can increase during pregnancy , worsens SDB. Keeping the room humid may help nasal passageways stay open.
- Consider raising the head of your bed by using bricks or risers. Because sleeping horizontally exacerbates sleep apnea, even a mild incline can ease SDB .
- Under the guidance of your doctor, consider using a CPAP machine. This device used during sleep is considered to be the gold standard for sleep apnea. It works by pumping air into the lungs and helping keep your airway open, ensuring a healthy supply of oxygen.
If you think you may have sleep disordered breathing, consult your doctor. Proper medical guidance is key for controlling this condition.
Soothe Your Legs
Pregnant women are more likely to experience leg cramping at night , caused by changes in the body’s ability to process calcium. Restless legs syndrome , a condition characterized by strong urges to move your legs, may occur more frequently in pregnancy
Try these techniques to prevent your legs from keeping you awake at night:
- Perform gentle leg stretches before bed.
- Get plenty of daytime exercise.
- Eat a calcium-rich diet.
- For sudden cramps, flex your feet or press them against the foot of the bed.
Ease New Parent Worries
While pregnancy is often an exciting, special time, it can also be filled with stress. Pregnant moms may lie awake ruminating about childbirth, the baby’s health, finances, or a number of other things. They may also experience nightmares and vivid dreams, which are common in pregnancy.
To cope with nighttime worry, try incorporating calming practices into your schedule, like yoga, journaling, and breathing exercises. Consider taking a soothing bath or practicing meditation to wind down in the evenings. You might sign up for a new-parent class to help prepare for the changes ahead. It may also be beneficial to reach out for professional support from a licensed counselor or support group. Many women are experiencing the same feelings, and seeking outside help can make a meaningful difference.
Avoid Sleep Aids
While it’s tempting to reach for a pharmaceutical or herbal supplement to combat sleeplessness, these products are usually not recommended for pregnant women. Sleep aids come with side effects, and they have limited research in pregnant populations. Even an over-the-counter antihistamine like diphenhydramine should not be used without consulting a doctor. Their effectiveness is unreliable, and there’s not enough evidence to be sure that sleep aids don’t adversely affect birth outcomes.
When in Doubt, See the Doctor
Don’t hesitate to seek professional advice for any change in sleep habits, no matter how small. While sleeping troubles can often be managed at home, sometimes a medical expert is needed to guide care or assess for something serious. Staying healthy is especially important during pregnancy, and good health starts with a good night’s sleep.
References
15 Sources
-
Chang, J. J., Pien, G. W., Duntley, S. P., & Macones, G. A. (2010). Sleep deprivation during pregnancy and maternal and fetal outcomes: Is there a relationship?. Sleep Medicine Reviews, 14(2), 107–114.
https://pubmed.ncbi.nlm.nih.gov/19625199/ -
Gay, C. L., Richoux, S. E., Beebe, K. R., & Lee, K. A. (2017). Sleep disruption and duration in late pregnancy is associated with excess gestational weight gain among overweight and obese women. Birth, 44(2), 173–180.
https://pubmed.ncbi.nlm.nih.gov/28198036/ -
Harskamp-van Ginkel, M. W., Ierodiakonou, D., Margetaki, K., Vafeiadi, M., Karachaliou, M., Kogevinas, M., Vrijkotte, T., & Chatzi, L. (2020). Gestational sleep deprivation is associated with higher offspring body mass index and blood pressure. Sleep, 43(12), zsaa110.
https://pubmed.ncbi.nlm.nih.gov/32496519/ -
Warland, J., Dorrian, J., Kember, A. J., Phillips, C., Borazjani, A., Morrison, J. L., & O’Brien, L. M. (2018). Modifying maternal sleep position in late pregnancy through positional therapy: A feasibility study. Journal of Clinical Sleep Medicine, 14(8), 1387–1397.
https://pubmed.ncbi.nlm.nih.gov/30092890/ -
A.D.A.M. Medical Encyclopedia. (2020, June 2). Problems sleeping during pregnancy. MedlinePlus., Retrieved April 1, 2021, from
https://medlineplus.gov/ency/patientinstructions/000559.htm -
O’Brien, L. M., & Warland, J. (2014). Typical sleep positions in pregnant women. Early Human Development, 90(6), 315–317.
https://pubmed.ncbi.nlm.nih.gov/24661447/ -
A.D.A.M. Medical Encyclopedia. (2019, January 19). Heartburn. MedlinePlus.
https://medlineplus.gov/ency/article/003114.htm -
Rhee, J., Kim, R., Kim, Y., Tam, M., Lai, Y., Keum, N., & Oldenburg, C. E. (2015). Maternal caffeine consumption during pregnancy and risk of low birth weight: A dose-response meta-analysis of observational studies. PloS One, 10(7), e0132334.
https://pubmed.ncbi.nlm.nih.gov/26193706/ -
Izci Balserak B. (2015). Sleep disordered breathing in pregnancy. Breathe, 11(4), 268–277.
https://pubmed.ncbi.nlm.nih.gov/27064321/ -
Artal-Mittelmark, R. (2019, July). Physiology of pregnancy. Merck Manual Professional Version., Retrieved April 1, 2021, from
https://www.merckmanuals.com/professional/gynecology-and-obstetrics/approach-to-the-pregnant-woman-and-prenatal-care/physiology-of-pregnancy -
Souza, F., Genta, P. R., de Souza Filho, A. J., Wellman, A., & Lorenzi-Filho, G. (2017). The influence of head-of-bed elevation in patients with obstructive sleep apnea. Sleep & breathing = Schlaf & Atmung, 21(4), 815–820.
https://pubmed.ncbi.nlm.nih.gov/28647854/ -
A.D.A.M. Medical Encyclopedia. (2020, January 29). Obstructive sleep apnea – adults. MedlinePlus., Retrieved April 1, 2021, from
https://medlineplus.gov/ency/article/000811.htm -
Office on Women’s Health. (2019, January 30). Body changes and discomforts. Womenshealth.gov.
https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/body-changes-and-discomforts -
A.D.A.M. Medical Encyclopedia. (2019, June 23). Restless legs syndrome. MedlinePlus., Retrieved April 1, 2021, from
https://medlineplus.gov/ency/article/000807.htm -
Okun, M. L., Ebert, R., & Saini, B. (2015). A review of sleep-promoting medications used in pregnancy. American Journal of Obstetrics and Gynecology, 212(4), 428–441.
https://pubmed.ncbi.nlm.nih.gov/25448509/










